PH WINS for All
- By: Lisa Tobe, MPH, MFA and Lauren Milliken, MSW, MPH
- Date
Including the Rural Public Health Workforce
Rural health departments remain understudied and underfunded — despite their importance in protecting the community’s health. Rural populations face increasing disparities in many health-related outcomes compared to urban communities. For instance, early COVID-19 pandemic infection rates rose more quickly in many rural communities and decreased more slowly after surges.
Rural areas often have limited health-related infrastructure and services, and local health departments can find it challenging to meet the health and wellness needs of their community.
Until recently, information about the rural public health workforce has been limited, making it difficult to identify ways these organizations can develop their staff. The PH WINS for All pilot sought to address this information vacuum by including small local health departments (LHDs)—organizations with fewer than 25 employees and/or serving less than 25,000 people—in PH WINS for the first time since its inception in 2014.
PH WINS, a nationally representative survey administered by the de Beaumont Foundation and the Association of State and Territorial Health Officials (ASTHO), examines local and state health department workers’ demographics, job satisfaction, engagement with public health issues, training needs, and more. Small health departments were previously excluded from PH WINS because of their limited capacity to obtain a representative sample and small sample size issues. Leveraging partnerships with two Public Health Training Centers (PHTCs), the PH WINS for All pilot was able to overcome previous barriers to conducting research in rural areas — the resulting data provide many insights about this unique segment of the national public health workforce.
Collaborative Efforts
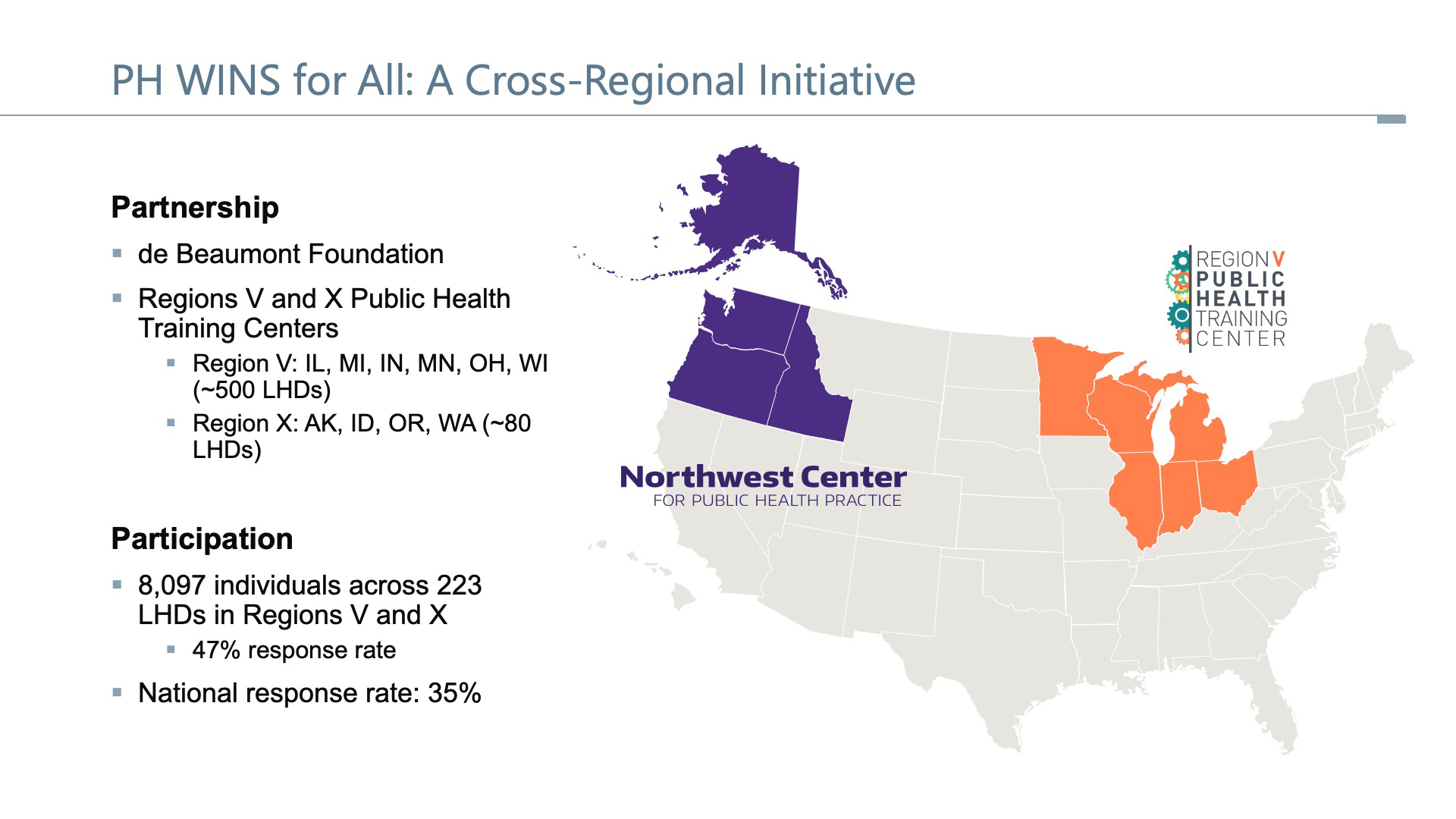
The PH WINS for All pilot engaged PHTCs housed at the University of Michigan School of Public Health Region V Public Health Training Center (PHTC) and the University of Washington’s Northwest Center for Public Health Practice (the Region X PHTC). Region V includes six states (Illinois, Indiana, Michigan, Minnesota, Ohio, and Wisconsin) and approximately 500 LHDs. Region X includes four predominantly rural states (Alaska, Idaho, Oregon, and Washington) and approximately 80 LHDs. Both PHTCs have a long history of community engagement and trust building at the local level, making them ideal partners for the pilot initiative. They are also members of the Public Health Training Center Network (PHTCN), a consortium of regional Public Health Training Centers that helps sustain a skilled public health workforce by providing access to world-class professional development, experiential learning, and consulting and technical assistance.
Betty Bekemeier, Ph.D., MPH, RN, director of the Northwest Center for Public Health Practice, knew how much the information gap regarding the rural public health workforce hinders LHDs’ ability to effectively use their assets to address local needs. The lack of rural data also limits the information available to tailor support to rural public health practitioners offered by the Regional Public Health Training Centers nationwide. Through what Bekemeier termed “a labor of love,” staff from the Region V and Region X PHTCs partnered with the de Beaumont Foundation to expand PH WINS data collection efforts and pilot a version of PH WINS that included small LHDs.
The partnership paid off, as is evident in the pilot’s higher LHD response rate overall for Region V and Region X than elsewhere in the nation. For small health departments, an increase in the number of LHDs and individual responses corrected previously mentioned sampling issues. Region V and Region X had a higher LHD response rate overall than the national response rates (47% compared to 35%). Over 200 (223) LHDs participated, enabling the PHTCs to gather insights from 11,016 respondents. This data can be used to advance collaborative efforts to transform the public health workforce and the infrastructure that supports it.
At the outset of the project, Region V and Region X began an intensive collaborative communications effort across ten states and approximately 580 local health departments. The de Beaumont Foundation provided recruitment messaging and FAQ templates. PHTC staff garnered commitments from health officials, identified workforce champions, organized staff lists, engaged partners, hosted virtual meetings, and developed mechanisms for tracking outreach, commitments, and contacts. Jointly, all involved organizations were able to accomplish what one could not do alone.
Results
The PH WINS data revealed several interesting trends and themes for small and mid-sized LHDs. Staff in small LHDs were more likely to be white (89%), while large LHDs’ staff were three times more likely to identify as Black, Indigenous, and People of Color (BIPOC) (37%). Public health professionals in small LHDs were more than two times less likely to have an advanced degree in public health and tended to have shorter tenures than professionals in large LHDs.
| Table X: Comparing National Samples with Region V & X | ||||
|---|---|---|---|---|
| National | Regions V and X Combined |
|||
| All | Small* | Large* | ||
| Female | 79% | 81% | 86% | 79% |
| 50 or younger | 62% | 66% | 65% | 68% |
| Tenure public health practice > 5 | 64% | 62% | 56% | 63% |
| Job class – public health sciences | 42% | 45% | 34% | 45% |
| BIPOC | 45% | 25% | 11% | 37% |
| White | 55% | 75% | 89% | 63% |
| Advanced degree | 36% | 18% | 18% | 39% |
| Some public health degree | 14% | 35% | 8% | 14% |
| 25K **Serving more than 250K | ||||
 As data collection partners, Region V and Region X PHTC have been able to parse the data in the context of rural health departments. According to research from Kett, Bekemeier, and Patterson (2023, in press[i]), rural staff had greater odds of reporting competencies related to community engagement, cross-sectoral partnerships, and systems and strategic thinking.
As data collection partners, Region V and Region X PHTC have been able to parse the data in the context of rural health departments. According to research from Kett, Bekemeier, and Patterson (2023, in press[i]), rural staff had greater odds of reporting competencies related to community engagement, cross-sectoral partnerships, and systems and strategic thinking.
In contrast, rural staff reported greater training needs related to data-based decision-making and justice, diversity, equity, and inclusion (JEDI). Bekemeier believes public health practitioners can leverage the community engagement and partnership strengths of rural public health staff to share with the broader workforce. This information enables PHTCs and other training entities to use this workforce development data to develop responsive training content driven by state and local needs.
“In a rural public health department, you may find yourself as the only person of color or the only LGBTQ person, which can be lonely,” said Bekemeier. “The Public Health Training Centers are looking at ways of connecting people across agencies in these rural areas so that [staff] remain, thrive, grow and contribute instead of feeling frustrated, lonely, or unsupported.”
PHTC staff have long been working with state and local health departments to use data to inform responsive workforce development that addresses employees’ cultural and capacity-building needs, help prioritize resource allocation, advocate for mental health support, and facilitate conversations. Bekemeier and other members of the Public Health Training Center Network are advocating for expanding the PH WINS for All pilot project to help public health agencies and training partners in other parts of the country better understand the unique local public health workforce needs in their regions. The PH WINS for All pilot project has demonstrated the effectiveness of the partnership between PHTCs, de Beaumont, and ASTHO. Through this effort, LHDs and organizations supporting them have access to richer and more comprehensive data to inform public health practice.
Resources
Robins, Moriah MPH; Leider, Jonathon P. PhD; Schaffer, Kay MPH; Gambatese, Melissa MPH; Allen, Elizabeth MS; Hare Bork, Rachel PhD. PH WINS 2021 Methodology Report. Journal of Public Health Management and Practice 29(Supplement 1):p S35-S44, January/February 2023. | DOI: 10.1097/PHH.0000000000001632
Kulik, Phoebe K. G. MPH, CHES; Leider, Jonathon P. PhD; Rogers, Megan MS; Karnik, Harshada PhD, MS, MPP; Power, Laura E. MD, MPH; Schaffer, Kay MPH; Bekemeier, Betty PhD, MPH, RN, FAAN. PH WINS for All: The Critical Role of Partnerships for Engaging All Local Health Departments in the Public Health Workforce Interests and Needs Survey. Journal of Public Health Management and Practice 29(Supplement 1):p S48-S53, January/February 2023. | DOI: 10.1097/PHH.0000000000001635
[i] Kett, P., Bekemeier, B., & Patterson, D. (2023, in press). Differences in competencies, training needs, and turnover risk among rural local public health practitioners compared to their urban peers: Findings from the 2021 Public Health Workforce Interest and Needs Survey. American Journal of Public Health.

 Subscribe To Our Communications
Subscribe To Our Communications